Transforming Conversations Around Black Maternal Health
Dr. Rachel Chapman is an activist, artist, poet, and associate professor at the University of Washington. She has over 20 years of experience studying health systems and teaching about the disparities within.
Throughout that time, Dr. Chapman has witnessed the widespread inequities in access to care, delivery of care, and resultant mistrust of the medical system for marginalized communities. Dr. Chapman says she has also seen a pattern of healthcare providers dismissing Black people when they talk about their pain. She knows first-hand how hard it can be to advocate for yourself in a medical setting.
“You’re sort of, in some ways, purposefully immobilized. Everyone else is the expert.”
Over the last two decades, since Dr. Chapman earned her PhD, serious concerns for maternal health in the United States have come to light. Between 1999 and 2019, the number of women who died within a year of pregnancy more than doubled, with the highest rates of death among Black women. According to the CDC, 80% of these deaths were preventable.
The release of this data has been vital to mobilizing researchers, medical providers, health & activist organizations, and academics to find solutions- Dr. Chapman among them.
While increasing efforts to protect marginalized women from dangerous pregnancy-related health outcomes is creating change- the widespread, necessary concern over the safety of black mothers and black expectant mothers has had an unintended consequence.
“What if telling someone they are a risk makes them more likely to be hurt?”
Heart & Soul Project
Over the last few years, Dr. Chapman has worked alongside a team of researchers, students, grassroots organizations, and medical professionals to bridge gaps in care for minoritized communities in and around Seattle.
First, the University of Washington partnered with the Somali Health Board of Tukwila to create Mama Amaan. Starting in 2019, they worked to bring holistic perinatal care directly to communities in several different East African languages.
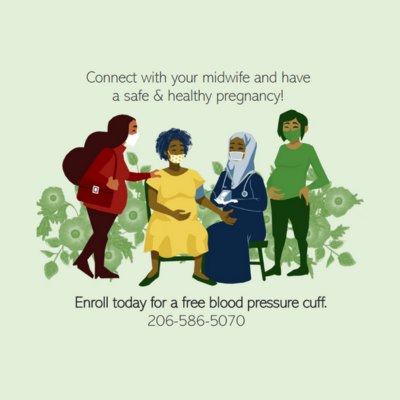
Photo from Mama Amaan.
In 2020, as in-person perinatal care shut down with the onset of the Covid-19 Pandemic, they pivoted. The work transformed into the first iteration of the Heart & Soul Project. The project provided over 100 pregnant women an at-home self-assessment kit. Using the provided blood pressure cuff and visual tool, mothers-to-be could evaluate their emotional and physical state every day based on a three-color system: green, yellow, and red.
Art by Jan Jimenez, UW Alum & Medical Student.
The Heart & Soul team encouraged participants to reach out to their care providers whenever their self-assessment landed in the yellow or red zone. Researchers found that participants reached out to their care team more often and with greater confidence than they otherwise would have. In some cases, Dr. Chapman says, the toolkit saved lives.
“It’s a beginning to talk with providers who serve communities with the greatest health needs about how they can center the wisdom of communities that don’t have a lot of power.”
Putting Joy First
During the project, researchers also learned something important. While doing the work to check in on mothers-to-be and ensure their physical and emotional well-being, conversations centered on risk-- and that weighed heavily on both participants and researchers.
“We were involved in this pathologization, and it was also affecting our bodies… So we decided... we have to front joy.”
The result of this discovery is their latest endeavor, Heart, Soul, & Joy.
In Heart, Soul, & Joy the team has added in a “Joy Quotient,” it’s an additional tool that encourages mothers-to-be to consider what is bringing them joy that day.
“People pick up the tool and they just light up.”
All internal meetings also begin with a Joy practice which can be as simple as asking “What are you looking forward to this weekend?” Dr. Chapman says it has improved their research practices as well.
“Our bodies, as we know, can produce a lot of immunity… Hope.. prayer.. are health-boosting, health amplifying… Maybe there’s something physical about not being made a problem.”
What’s next?
Dr. Chapman explains that the responsibility for changing systems does not lie with the already overstretched medical professionals working in community-based clinics.
“People in public clinics, in community clinics are doing the heaviest lifting with the least resources.”
The goal is to demonstrate how a small package of care, offered to all people regardless of location, income-level, or insurance, can improve health outcomes. As the team continues to gather data, they hope to encourage policy changes that allot more Medicaid dollars to a similar, more comprehensive health packages for all pregnant people.
Heart, Soul, & Joy thanks their partners:
East African communities and birthworkers of Seattle, NeighborCare Health Clinics, HealthPoint Health Systems, Mama AMAAN and Heart Soul & Joy Research Teams, especially Jihan Rashid, Somali Health Board, Drs. Ahmed Abdille, Muna Osman, Health Alliance International, Julia Robinson, James Pfeiffer, Parent Trust, Sally Brady, University of Washington: Royalty Research Fund, Population Health Initiative, Department of Anthropology, Global Health, School of Public Health, Psychiatry, School of Social Work, Pediatrics, CSDE
This year, April 11th through April 17th marked Black Maternal Health Week. It was started by an organization called “Black Mamas Matter,” held intentionally during Minority Health Month to call attention to the disparities in dangerous pregnancy-related health outcomes for black women.
ABOUT THE WASHINGTON STATE WOMEN’S COMMISSION
The Washington State Women’s Commission, created by the Washington State Legislature in 2018, aims to improve the well-being of women by identifying and developing policies to remove systemic barriers and address critical issues that disproportionately impact women, including childcare access and affordability, domestic and gender-based violence, equal pay, and intersectional inequities.
Learn more at wswc.wa.gov.